Reports from VIV Europe 2018
‘There is no need for pessimism about antibiotic resistance’

The University of Ghent researcher, and the principal author of the annual Belgian report on antimicrobials in animals (BelVet-SAC), has just published a guide, 8 Myths on Antibiotic Resistance Disproved, with several objectives, perhaps the main one being to show farmers how to reduce their reliance on antibiotics in a smart, economically viable way.
He believes that antibiotic resistance “should not be looked at as a threat, but rather as an opportunity to reach the next level of a high quality and sustainable animal production system.”
Misunderstandings
We spoke to him at VIV Europe 2018 in the Netherlands to understand why he saw fit to publish the book.
“My research group has being doing work on both antibiotic usage and antibiotic resistance and biosecurity for about 15 years. And when I give presentations on the topic [in a myriad of countries], I recognize there are a lot of misunderstandings.
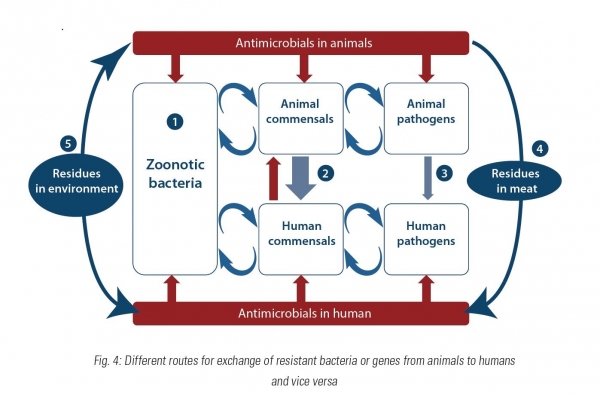
“People [both the general public and farmers] have some preconceived ideas that are not fully in line with what is going on. For example, there are a lot of misconceptions on how antibiotic resistant bacteria can go from animals to humans – and it is possible that they go from animals to humans – mostly people think this happens by consuming meat or drinking milk but all the studies available would indicate that direct contact with animals is a much more risky activity than consuming meat or drinking milk [in this regard] – that is one of the myths that I tried to debunk.”
He said one other misconception farmers have is that reducing antibiotics in their production will automatically cost them money, with such financial outlay coming on top of what they have already paid out in order to be compliant with new welfare legislation, for example.
“I try to explain, based on a lot of research we have done, that you can improve situations, you can make things better without having additional costs, by simply improving your management, your biosecurity, and that these approaches can give you a positive return. There are some small investments that you have to make to ensure better biosecurity but they pay off in two ways - you can use fewer antibiotics and you can improve your overall production results. I have documented that approach in the book.”
'The main driver for resistance is use'
The first part of the book explains that antibiotic resistance is a real risk and how it is a very complex issue. The second part looks at how the livestock industry might go about solving the problem.
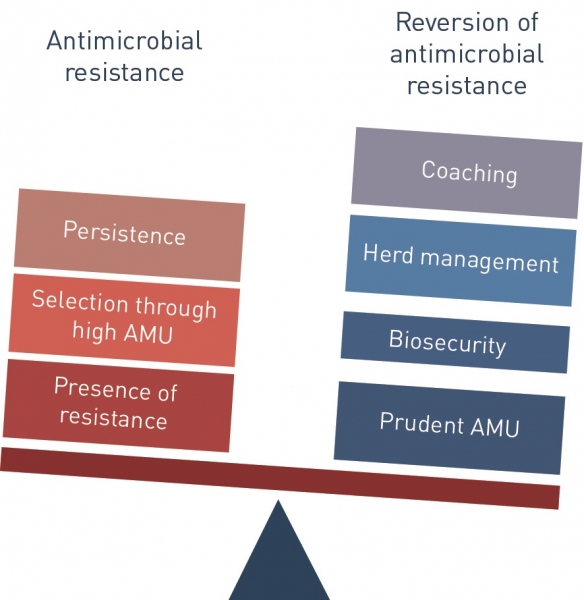
“We in animal production have a responsibility. The main driver for resistance is use. The more antibiotics you use the more the resistance you have. But the good thing is that the fewer antibiotics you use the less resistance you have. It is reversible.”
He cites the declining level of resistance in Belgium and in the Netherlands, both countries which have seen a reduction in farm antibiotic usage in recent years, as evidence of this reversibility. “That is very hopeful. That shows that trying to do something about this actually pays off.”
"Right at the start, we can already bust one resistant myth: antibiotic resistance is not worth losing any sleep over. Wrong."
"More and more, doctors come across bacteria that have become resistant to all types of drugs. Sadly, these superbugs are no urban myth.... Resistance genes are emerging and spreading all over the world at an alarming rate, threatening to throw our society back into the pre-antibiotic healthcare era, where common infectious diseases were hard to treat and could even lead to death."
"Estimates reveal that antibiotic resistance, as we speak, already results in an additional health care cost of €1.5bn per year in the European Union."
- Extracts from 8 Myths on Antibiotic Resistance Disproved
“It is not the case that we can say tomorrow everybody should stop using antibiotic treatment in piglets post weaning. But ultimately we should get to the point where you can wean piglets without having to rely on antibiotics except for the incidental disease outbreaks. But all this preventative and systematic use is the type of use that we need to get rid of - not in one step, not tomorrow, and not for everybody immediately.
“You need to give the farmer some time and that is what I explain in the book.”
Check, improve and reduce
He said first producers need to check, improve and reduce.
“You need to do it in that order. You have to check the situation – what your level of biosecurity is, what your quality of feed is. Secondly, you have to improve a number of things – hygiene, perhaps the feed or the water quality – whatever is suboptimal. Then you can go to the step of reducing the use of antibiotics. If you don’t follow those steps, you will run into problems.”
He said he is not an advocate of replacing antibiotics with other medicines. “Sometimes improved vaccination is good but it is not all about more vaccines. It can also be about better feed and not necessarily more expensive feed. We have guided a lot of farmers in this process of reducing antibiotic use and what we have seen is that if they feed in a slightly less intensive way during the early stages after weaning, the piglets catch up some weeks later, and they get to the same growth curves at the end. They are just managed a bit differently. At the moment the animals are vulnerable, that they are stressed, you shouldn’t push them too much. You need to give them a bit more time.”
In that context, he also offers advice in terms of the optimal weaning age for piglets:
“There are a lot of countries that are moving to weaning at three weeks which, in my opinion, is not a good idea. It is too early. It is better to try and organize a system where you wean at four weeks, or at 25 or 26 days, but not earlier. If done in an optimal way, it doesn’t have to cost you money, If done in a smart way, such a system won’t have a negative effect on final production returns.”
Anyone who wants to get hold of the publication needs to get in touch with the author, Jeroen Dewulf, directly. He is based at the Veterinary Epidemiology Unit, Department of Reproduction, Obstetrics and Herd Health, Faculty of Veterinary Medicine, Ghent University. His contact details are oniine.
It is about changing the mindset and giving farmers assurance and tools, he said.
“When you treat animals with antibiotics things can also go wrong. There are plenty of studies showing higher mortality on farms that use a lot of antibiotics, more disease pressure on such farms than on ones with more limited antibiotic application. When you take away the umbrella of antibiotics, your management mistakes become a lot more obvious.”
Markets beyond Europe are embracing this idea of the need to migrate away from antibiotics, he added.
“Lots of countries are moving in the right direction. Two years ago I would have said it was mainly Europe, but now it also the rest of the world is catching up. There is a lot of interest in the topic in Asia now, whereas four or five years ago they didn’t want to hear about it.”
It can go fast, particularly if all the actors involved in meat production are on the same page, he said.